How to Fix Benefits Administration M&A Payments Pain
M&A has major implications for benefits administrators—and payments infrastructure shouldn’t be an afterthought.

Mergers and acquisitions (M&A) are a driving force across the healthcare industry, with continued impact on the benefits administration space. Recent examples include the expansion of Optum and HealthEquity’s acquisition of both Further, a provider of HSA and consumer-directed benefit (CDB) admin services, and BenefitWallet’s HSA portfolio.
Acquisitions enable benefit administration companies to enhance service offerings, expand their geographic footprint, enable cost efficiencies, and implement newer technologies. As scale increases, these businesses can run into a host of challenges, especially around money movement. Similar to companies across healthcare, benefits administration involves complex systems and sensitive high-volume data, marked by the persistence of legacy systems. M&A activity is likely to compound these issues because much of this activity happens without a plan for how to centralize and normalize payment operations infrastructure.
Trends in Benefits Administration
Several factors influencing the benefits administration industry provide context for the demands on payments infrastructure post-M&A.
Trend: Industry consolidation and bundled services
Result: Growth-oriented benefits administrators may operate using a variety of financial systems, as well as manual reconciliation.
The healthcare benefits industry is undergoing significant consolidation in tandem with increasing pressure to offer bundled services. According to recent data, the top two priorities for employers regarding benefits are managing healthcare costs and trends, and the ability to attract and retain employees.
The latter entails providing access to healthcare savings—via employee health benefit accounts like health savings accounts (HSAs)—and comprehensive wellness benefits that extend to mental health. The ability for benefits administrators to diversify offerings is a significant driver for M&A activity. The desire to create a “one-stop-shop” is also fueling price compression and tighter profit margins, especially for HSAs.
Trend: New business lines
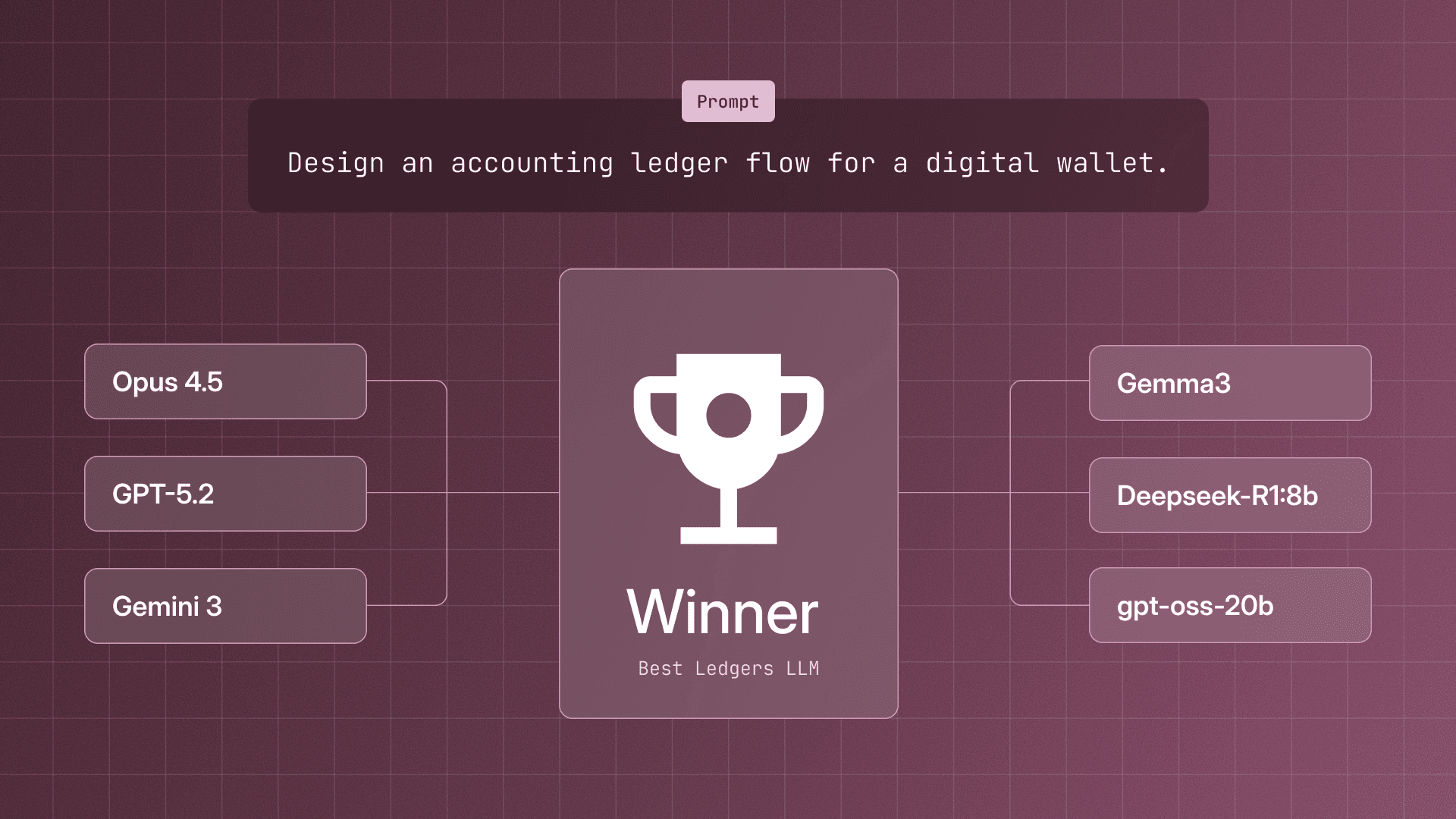
Result: New product offerings require new partnerships and capabilities—for example, a robust core ledger system is essential for enabling healthcare lending services.
Benefits administrators are expanding their investments to include healthcare lending and lifestyle savings accounts (LSAs). Healthcare lending involves offering competitive loans to healthcare providers such as hospitals and dental offices. Benefits administration companies are expanding into LSAs due to potentially higher margins and less regulatory scrutiny. These businesses are also partnering with major marketplaces and brands—these partnerships and expansion into LSA marketplaces can result in potential funds tracking and reconciliation challenges.
There’s also the ongoing expansion of major companies into the healthcare and benefits industry. Amazon continues to grow its healthcare offerings, building on top of existing partnerships with Oracle, One Medical, and others. These services, as well as those offered by brands like Uber and Walmart, put additional pressure on providers, payers, and benefits administrators when it comes to competing via new business lines.

Payments Infrastructure and Pain Points After M&A
M&A activity and the pressure to expand offerings can amplify existing payments challenges in benefits administration. Pain points include:
Disparate systems
Mergers and acquisitions can compound problems that arise from already inconsistent, sprawling financial systems. The more acquisitions a company makes, the more financial systems need to be stitched together. As an example, a company might operate with its record-keeping and administration on separate platforms, necessitating frequent file exchanges to ensure accurate transaction records. The resulting manual reconciliation processes could wind up consuming valuable time and resources.
Manual processes
In benefits administration, manual workflows hamper auditability, which has significant implications for risk and security. Lacking real-time insight and reconciliation makes it harder to launch new products and grow revenue. Repetitive tasks tend to increase the likelihood of errors—insight into transaction settlements, approvals, and balance updates is also limited, hampering confidence. Automated money movement can streamline manual data entry processes, cut operational costs, and boost efficiency and accuracy
Reconciliation and settlement challenges
Certain health benefit account types introduce particular tracking complexity. HSAs are fully loaded for individual consumers at the beginning of the year. The consumer then pays into the account with each paycheck. This setup presents reconciliation complexities, as funds need to be matched while the consumer spends down the account.
Errors can be costly for administrators—not only because poor consumer experience can potentially decrease HSA adoption, but also due to the operational expense of manual reconciliation errors that necessitate spending to cover unaccounted transactions. Certain benefit companies also face significant difficulties with transaction settlement. When businesses batch ACH payments as a result of legacy systems, for example, it can be difficult to identify individual erroneous transactions.
Choosing Between Build or Buy
In light of these challenges, growing benefits administrators must ultimately choose between building a native solution or partnering with a third-party if they want their infrastructure to stay competitive. Given the intricacies of their joined systems, combined with complicated industry-specific regulations, businesses often choose to build in-house.
Building payments infrastructure that can manage bank payments at scale—or rebuilding and centralizing systems, as the case may be—is resource-intensive. Primary costs include personnel (not just engineering but also product, operations, finance, and treasury), payment and bank fees, and technology. The latter can involve an extensive investments for functionality including:
- Initiating and receiving payments, with the ability to handle file standards such as NACHA, BA12, ISO20022, MT940, etc.
- Handling ACH returns and reversals, which requires return file parsing, reversal functionality, and the ability to initiate a return
- Onboarding counterparties, including collecting information, verifying accounts, and ensuring compliance
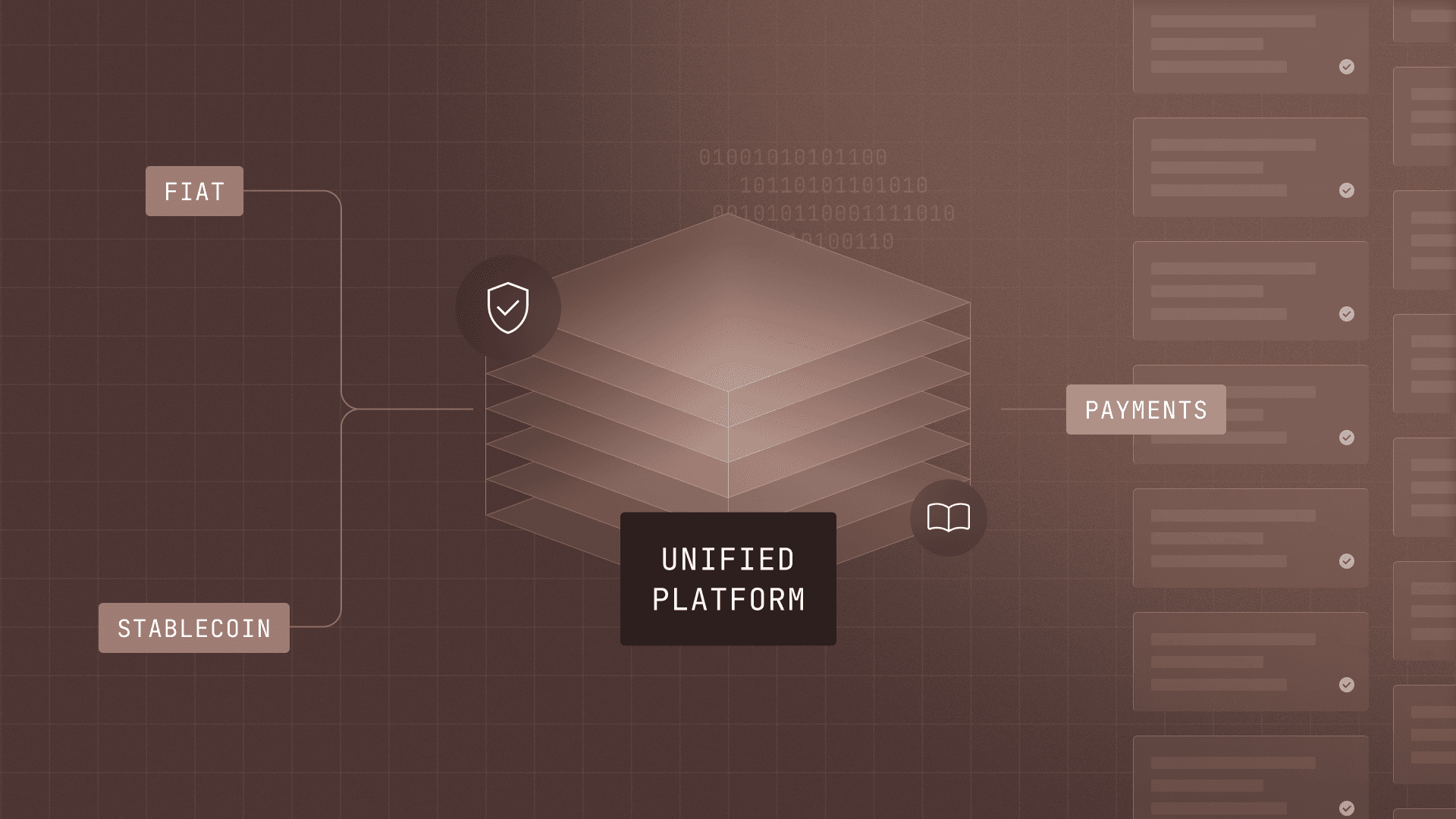
- Enabling automatic reconciliation and continuous accounting, including the normalization of data across different file standards and integration with an ERP
- Supporting virtual accounts and a central, double-entry ledger database
- Providing controls that include role-based access, audit logging capabilities, and approval workflows
And if something goes wrong, the time and expense required to research, fix, or in the worst cases, pay out fines, may offset any potential benefits of building in-house.
Sana Benefits calculated these tradeoffs when making the choice to build or buy. For Sana, partnership proved a better investment. The team implemented Modern Treasury API calls with a few lines of code, enabling them to tag reconciled payments with the right accounting categories and attribute them to the right vendors and customers, continuously syncing that data to their data warehouse.
For benefits administrators, the right payments infrastructure solution can have significant benefits, including:
- Lower operational overhead and better control. Centralizing disparate financial systems resulting from M&A activity and legacy platforms can streamline time-consuming manual processes.
- The ability to launch new business lines faster. For technology providers looking to invest in new business lines, valuable resources can are better-focused on new products (not building or managing daily money movement workflows). Investment in robust ledgering infrastructure, for example, can help organizations stand up healthcare loans or CDH marketplaces much faster.
- Improved end-user experience. Users count on the ability to reliably access accurate balances in real time. This expectation requires that benefits administrators ensure complex payment transactions (as the account is spent down and funds paid into the system) are reconciled precisely, continuously, and adaptively.
A Customer Story
An enterprise health benefits provider for TPAs—managing $40M in money movement daily and 4 million transactions annually—needed to solve reconciliation challenges. Operating across siloed, fragmented systems had resulted in manual work and risk exposure, with the possibility of write-offs. By partnering with Modern Treasury, the company can now:
- Easily collect and attribute employee contributions
- Oversee reimbursement for employee out-of-pocket HSA purchases
- Orchestrate payment flows across 40+ bank accounts
- Automate complex bank account reconciliation (including real-time reconciliation on returns at scale)
- Save time during each accounting close
- Stay compliant for future audits
As a result of using Modern Treasury, this company has undergone significant, end-to-end digital transformation around payments and is pursuing further automation in partnership with our team.
The Right Partner for Benefits Administration Companies
Modern Treasury is the operating system for money movement, helping healthcare and benefits administration companies of all kinds process bank payments in-house, reduce overhead, and automate reconciliation. Reach out to learn more.